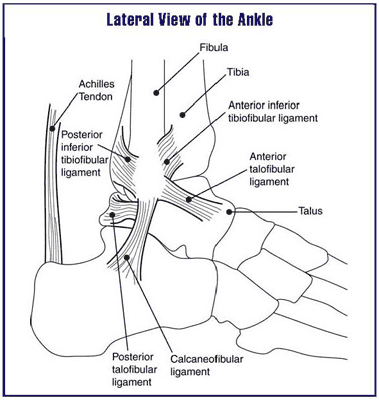
The ankle joint is made up of the bones of the lower leg, the tibia and the fibula, which rest on top of the ankle bone known as the talus. These bones are held together by strong ligaments that allow us to put several times our body weight through the joint whilst doing actions like running, jumping, twisting etc.
When an ankle sprain occurs, the ligaments around the joint become stretched and torn causing pain, swelling and can give the feeling of joint instability. But not all sprains are equal and the location and mechanism of injury can play a significant role in how your injury is managed.
What is a high ankle sprain and how is it different from a common ankle sprain?
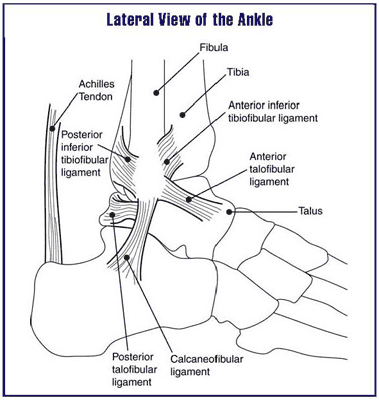
A high ankle sprain, also known as a syndesmotic injury, is an injury to the ligaments that hold the bones of the lower leg (tibia and fibula) together at the ankle joint. Together they are referred to as the syndesmosis ligaments but the anterior inferior tibiofibular ligament (AITFL) is the most commonly affected structure.
In contrast, a "common" ankle sprain, which is the more likely injury, involves disruption of the ligaments that hold the ankle bone (talus), to the lower leg bones.
The most common mechanism of injury for a high-ankle sprain is when someone falls or lands awkwardly on their foot whilst turning or performing a cutting motion. Hence it is a common occurrence in sports such as basketball, soccer, football, hockey, lacrosse, tennis and volleyball.
Due to the high energy normally required to cause a high ankle sprain this injury is usually associated with other foot and ankle injuries - osteochondral injuries (injuries to the surface of joints) occurs in 15-25% of cases.
What are the symptoms of a high ankle sprain?
A person who has sustained this kind of injury will often have difficulty walking because they cannot support their body weight on the injured limb. Depending on the severity of the injury, the pain may radiate up the leg from the ankle every time you try to take a step. This is because the tibiofibular joint will try to separate due to the syndesmotic ligaments holding them together no longer functioning.
There may be very little swelling around the ankle following a high ankle sprain so it is easy to underestimate the severity of an injury.
On clinical evaluation, the location of your pain may be focused on an area just above the ankle joint line.
How to treat a high ankle sprain?
To know how to best manage your injury, we will first need to know the severity. This means you will undergo investigations such as weight-bearing x-rays (not always a pleasant experience soon after an injury) and MRI scans of the ankle joint.
Treatment depends upon the degree of damage caused by the initial trauma. If there is only minor soft tissue damage then immobilisation using a boot or cast could suffice. However, if there is significant structural damage to the ligamentous structures then surgery will need to be considered otherwise you risk getting complications of chronic ankle instability.
Once the syndesmosis joint is stable, you will undergo physical therapy to help restore your ankle function.
How long does it take to recover from a high ankle sprain?
A low-grade high ankle sprain, treated non-operatively, can take anywhere between 6-8 weeks to recover from. However, if surgery is needed then recovery times, that is time to return to sports, can vary significantly. In some cases taking 3 months or longer.
If it is not properly treated, it can lead to long-term problems including, loss of ankle range of motion and developing ankle arthritis.
If you think you have sustained a high ankle sprain, you should arrange to see a doctor immediately. Click here to schedule an appointment.
Pain in the ball of your foot? Tingling and numbness in your toes? The constant feeling of a stone in your shoe? You may have a Morton's neuroma.
What is a neuroma?
A neuroma is a benign (non-cancerous) tumour of a peripheral nerve. They are often caused by nerve injuries such as direct pressure or repetitive trauma or can form at the end of a cut nerve. Less often multiple neuromas can form due to a genetic condition known as neurofibromatosis, but we will not be covering this.
What is Morton's neuroma?
Mortons' neuroma, first described by Thomas Morton in 1876, is a painful condition that affects the ball of the foot. Compression or irritation of a digital nerve in the space between the foot bones (intermetatarsal space), typically between the 2nd and 3rd or third and fourth toes, causes the sheath surrounding a nerve to become inflamed and over time develop into a lump.
What causes Morton's neuroma?
There are a number of risk factors that may predispose you to develop Morton's neuroma. All of these in essence cause compression or irritation of the digital nerve in the intermetatarsal space:
Footwear - One of the main offenders is wearing narrow shoes that stop your foot from expanding when you walk or high-heeled shoes that force your toes into the toe box.
Foot shape - Certain foot deformities like having a bunion, hammertoes, flat feet or having flexible feet increases your risk of developing a neuroma.
Exercise - High-impact activities like running, walking long distances on hard surfaces, or standing for long periods of time may not only cause a neuroma but if present will bring on the symptoms.
Weight - Carrying excessive weight, either in you (obesity) or on you (weights), puts additional stress on your feet.
What does Morton's neuroma feel like?
Typical neuroma symptoms people report is the feeling of having a marble or pebble in their shoe when there isn't one. You may get a pain in the ball of the foot when standing or walking. You may even experience tingling, burning or numbness in the toes. These symptoms tend to improve when you take off your footwear or you're off your feet.
Diagnosis of Morton's Neuroma
The diagnosis is made from your medical history and physical examination when we attempt to reproduce your symptoms.
Ultrasound imaging done during your appointment can confirm the position and size of a neuroma.
X-rays may be requested to look for other possible causes of foot pain like a metatarsal bone stress fracture or joint arthritis
Magnetic resonance imaging (MRI) is occasionally used in cases that have failed initial conservative management to look for other possible causes. The common alternative diagnosis is intermetatarsal bursitis, an enlarged fluid-filled sac in the same area causing irritation and inflammation of the nerve.
Treatment options for Morton's neuroma
More than 80% of people with Morton's neuroma will improve without the need for surgery.
The first line of treatment focuses on non-operative methods, many of which you can try yourself:
- Activity modification - Cut back on the activities that trigger your symptoms. ok to cut back
- Shoe modifications - Wide fitting shoes are preferable. Avoid wearing shoes with narrow toe boxes or high heels.
- See a podiatrist to provide padding or a custom orthotic/insoles to support the metatarsal arch to reduce pressure on the nerve.
- Injection - An injection is administered under ultrasound guidance into the fibrotic tissue around the nerve. The most common substrate used is a cortisone injection but alcohol injections are also done.
- Radiofrequency ablation or cryoablation - Burning or freezing the nerve to stop it from transmitting pain signals.
- Surgery - If you do not respond sufficiently to a non-surgical approach you will be referred to a foot and ankle surgeon to have a discussion about removing the neuroma.
It is best to see a specialist as soon as you start to get symptoms of Morton's neuroma. An early diagnosis lessens the need for more invasive treatments. Click here if you wish to schedule an appointment.
What is plantar fasciitis?
 Plantar fasciitis (plan·tuh fa·shee·ai·tuhs) is the most common cause of heel pain estimated to affect 1 in 10 of us at some point in our lives, and of these, roughly 1/3 will have it in both feet.
Plantar fasciitis (plan·tuh fa·shee·ai·tuhs) is the most common cause of heel pain estimated to affect 1 in 10 of us at some point in our lives, and of these, roughly 1/3 will have it in both feet.
The plantar fascia is a thick band of fibrous tissue that runs along the bottom of your foot from the heel bone (calcaneum) to your toes. It works like a tight rubber band to support the arch of your foot and shock absorption when you land your foot with each step. Repeated stretching and tearing can cause irritation or inflammation of the fascia, although the cause of fasciitis is not known in most cases.
Risk factors for developing plantar fasciitis
Even though there is no obvious cause, some factors can increase your risk of developing plantar fasciitis (PF). They include:
Age - PF can happen at any age but the highest occurrence is seen in individuals aged between 40 and 60 years. This may have to do with the plantar fascia becoming less like a rubber band as we age.
Weight - Up to 70% of patients with plantar fasciitis are overweight. Having a high body weight puts extra stress on your plantar fascia so, keeping a healthy weight can help prevent or resolve the problem.
Type of exercise - Similar to being overweight, weight-bearing activities that place a lot of stress on your heel - such as running, weight lifting, dancing, or skipping - may bring on the condition.
Foot mechanics - The mobility of your foot and ankle can be affected by you having flat feet, high arched feet, or tight calf muscles (tightness of the Achilles is found in over 80% of cases of PF). These affect how weight is distributed across your feet when you're upright which can contribute to your developing fasciitis.
![Heel spur]() Heel spur
Heel spur
Do heel spurs cause plantar fasciitis?
A heel spur is an outgrowth of bone from the weight-bearing area of the heel bone. It is normally a chance finding when an x-ray of the foot is done for other reasons.
Having a heel spur does not mean you will get pain from it. Less than half of cases with plantar fasciitis have a heel spur.
Symptoms of plantar fasciitis
Heel pain or pain in the arch of the foot that is worse getting up first thing in the morning or after a period of prolonged sitting. The pain can be bad enough to make your first couple of steps be taken gingerly. After a few minutes of walking, the pain decreases as the fascia is stretched.
Gradually worsening heel pain with prolonged periods of standing or walking long distances.
Diagnosing plantar fasciitis
Diagnosis is fairly straightforward from the medical history you provide and a thorough physical examination carried out by your physician. Further confirmation can be achieved with ultrasound imaging performed at your outpatient appointment.
Occasionally further imaging tests like a magnetic resonance imaging (MRI) scan may be requested to rule out other conditions that can present like PF.
During your clinical evaluation risk factors for developing PF will also be explored and, if necessary, addressed.
What else can cause heel pain?
It's important to appreciate that there are different causes of heel pain, other than plantar fasciitis. Conditions like:
- Calcaneal (heel bone) stress fracture
- Plantar fascia rupture/tear
- Heel fat pad atrophy/wasting
- Tarsal tunnel syndrome - a nerve entrapment syndrome.
Though rarer, it is important that these conditions don't get missed as some cases may require urgent medical attention.
Ignoring plantar fasciitis can lead to chronic heel pain that hinders your regular activities. Changing the way you walk as a way to relieve your foot pain might lead to further problems of the foot, knee, hip or back.
How do you treat plantar fasciitis?
Although it can be debilitating, take comfort in the knowledge that roughly 90% of cases of plantar fasciitis improve within 6 months with non-operative treatments. Examples of at-home remedies you can do include:
- Regular gentle stretching exercises targetting the calf muscles. This can be instructed by a physical therapist.
- Standing on a frozen water bottle or applying an ice pack to the painful area for 10 to 15 minutes three to four times a day
- Use a cushioned heel gel inside your shoes
- Wear supportive shoes. Some people find it more comfortable wearing a heel lift in their footwear.
For those cases that don't respond to early conservative treatment, further options include:
- Extracorporeal shockwave therapy (ESWT)
- Platelet Rich Plasma injection
- Getting shoe inserts following assessment by a podiatrist
- Corticosteroid injection - usually reserved as a last resort when all other methods have failed.
If you have heel pain that is affecting your quality of life
make an appointment to see Dr. Ade.
 Plantar fasciitis (plan·tuh fa·shee·ai·tuhs) is the most common cause of heel pain estimated to affect 1 in 10 of us at some point in our lives, and of these, roughly 1/3 will have it in both feet.
Plantar fasciitis (plan·tuh fa·shee·ai·tuhs) is the most common cause of heel pain estimated to affect 1 in 10 of us at some point in our lives, and of these, roughly 1/3 will have it in both feet.