“Painsomnia”, or the inability to sleep due to pain, is all too common for those who suffer from knee osteoarthritis. In fact, data from a 2020 study in collaboration with NHS Digital showed that searches for pain management on the NHS website peaked between 11 pm and 4 am and visits to pages describing musculoskeletal conditions peaked between 6 am and 7 am. We can assume from this search behaviour that people search for ways to control their pain when it's bothering them the most, and the following morning look for articles like this one to find out what the cause of their night pain is and how to stop it from happening again.
What causes knee pain?
Let's go back to basics. Cartilage is the soft tissue that covers the surfaces of bones inside the joints in our body. It allows the joints to move smoothly with little friction. The knee joint has additional specialised fibrocartilage known as the menisci (meniscus - singular) that has the added function of acting as a shock absorber. These spread the weight evenly across the joint surface whenever you move or load your knee preventing overloading of one area over another.
As we get older cartilage naturally degrades and loses its elasticity causing it to become stiffer and making it more susceptible to damage. It's this natural wear and tear that leads to irritation and inflammation of the joint lining causing such symptoms as pain and swelling associated with osteoarthritis.
Why is knee pain worse at night?

While there isn't a definitive answer to this question, it's likely due to a number of reasons:
Low night-time cortisol levels
Most people have heard of cortisol and how it is associated with increased levels of stress, but did you know that it is also a powerful anti-inflammatory?
Cortisol is a steroid hormone naturally produced by the body. It regulates how we process fats, carbohydrates and proteins. It regulates the body's immune system and how it responds to inflammation.
 Plasma cortisol levels over a 24 hour period. Images copyright of Encyclopedia Britannica.
Plasma cortisol levels over a 24 hour period. Images copyright of Encyclopedia Britannica.
The body's levels of cortisol fluctuate across the day peaking around 8 am and troughing somewhere between midnight and 4 am. Lower nighttime levels mean there is less naturally occurring anti-inflammatory circulating.
Another theory, summarised in this 2015 review, is that if you are under continuous stress such as from having a chronic inflammatory condition this may lead to the body producing generally less cortisol to counter the ongoing inflammation.
In either case, you will have an effectively lower level of naturally produced/endogenous anti-inflammatory during the early hours of the morning.
Daytime physical exertion
"If I've had a long day on my feet... I tend to feel the pain more at night, or the next day."
A common story I hear from patients with knee arthritis is that their pain worsens across the day or after a period of increased physical exertion. So it's normal for them to expect to have night-time pain following a particularly active day. But why is this the case?
Our understanding of what's happening in the process of osteoarthritis has changed over time. Previously, we believed that this was simply a "wear-and-tear" phenomenon that meant that given enough time and use all joints will wear out. But this does not explain why some runners with 1000s of miles behind them show little wear in their joints, whereas some individuals who've lived relatively sedentary lives develop significant arthritis.
We've now come to appreciate that there is a complex inflammatory process contributing to the degeneration occurring inside osteoarthritic joints. Increased activity on an already degenerative joint can lead to greater levels of pro-inflammatory mediators, which just so happens to reach peak concentration in the middle of the night.
Reduced night-time muscle tone
Muscles around the knee give it support and stability in everyday activities. When you are asleep these muscles relax in essence removing the support they are providing. Without this support, uncontrolled movement or unguarded positioning during sleep may aggravate structures inside and around a joint leading to pain.
Nothing is distracting you!
During the day, the hustle and bustle of life provide a welcome distraction from a painful joint but when you go to bed and things are quiet you may simply notice the pain more.
"Painsomnia" - The vicious cycle of night pain
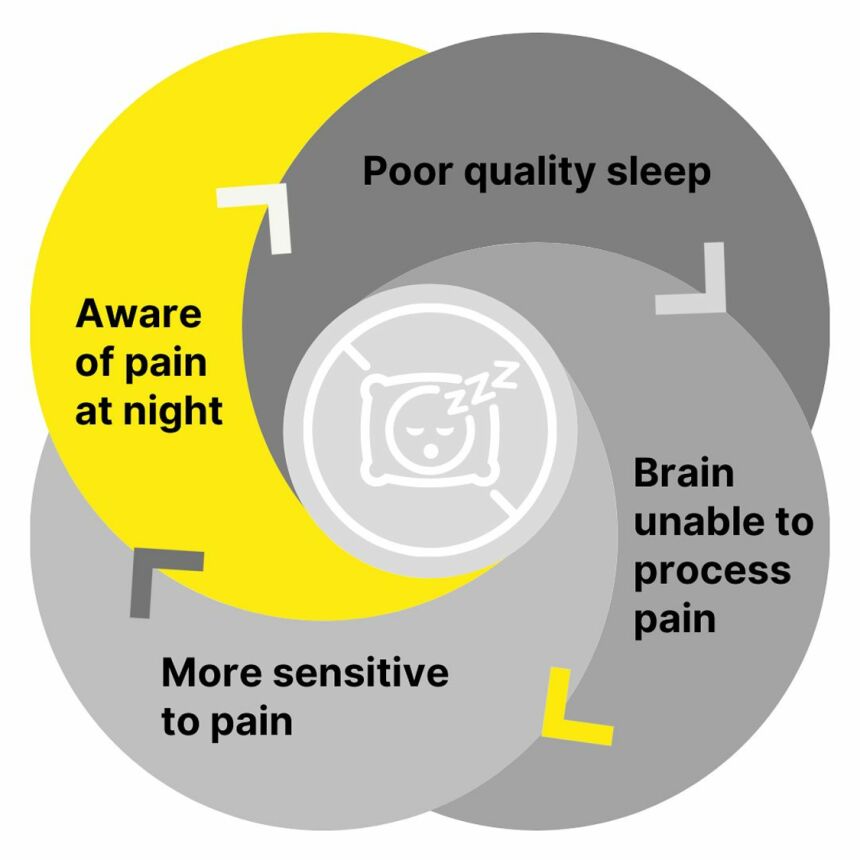
A study published in the Journal of Neuroscience in 2019 established that sleep deprivation has a direct effect on how our brain processes pain. When you suffer from short sleep times, if your sleep is fragmented or of poor quality, you become more sensitive to pain. What would be scored as a 3/10 may now be interpreted as a 5/10 level of pain.
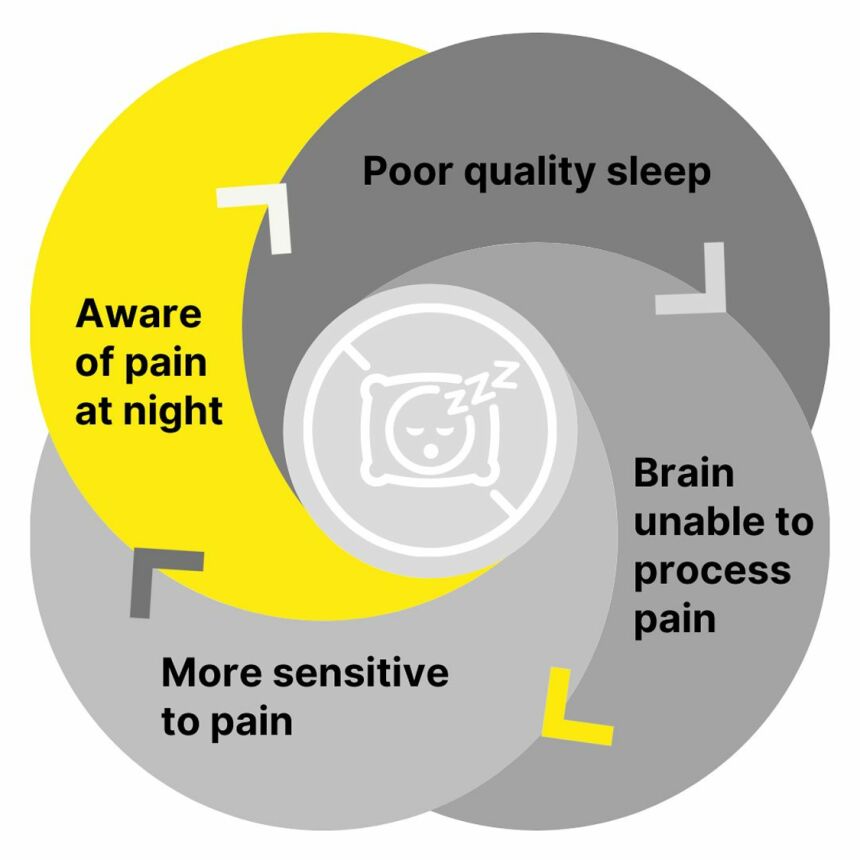
When you’re tired your brain becomes less able to dampen pain signals which leads to a heightened perception of pain. This in turn results in disturbed sleep and so on...
How to treat night-time knee pain
While you can’t cure osteoarthritis there are some things you can do to help you get better quality sleep:
Sleep hygiene - It might not seem so important but establishing a healthy sleep routine will help you to normalise your sleep pattern which will make it easier to contend with the disruptive effect of night-time pain.
- Go to bed early to allow a good length of sleep. Get up at the same time each day and avoid daytime naps
- Keep your bedroom cool and dark
- Avoid screens at bedtime particularly blue light from phone screens
- Avoid caffeinated drinks (tea, coffee, energy drinks)
- Don't exercise or eat heavy foods close to bedtime
Timing your pain medication - Take a slow-release pain killer that works through the night or take your night dose just before bedtime. Work with your doctor to make sure any adjustments to your medication fits with your treatment plan.
Relaxation/meditation - If you are woken up by pain try meditating, visualisation or whatever relaxation technique you may be comfortable with. If this does not work try reading a book in a quiet room, avoiding bright light. Scrolling through your social media feed is not advisable.
Pillow positioning. If you sleep on your side you can try to sleep with a pillow between your knees. If on your back try placing the pillow under your knees.
Try to stay active - Regularly exercising improves pain, swelling, and stiffness associated with arthritic joints. People who exercise regularly have lower levels of pain overall. This is why I routinely recommend physical therapy as part of my strategy for managing osteoarthritis.
The difficulty is finding the right balance between rest, what type of exercise and how hard you can go at it without causing a flare-up of your pain.
Consider getting psychological support - Cognitive behavioural therapy or CBT can provide long-lasting benefits for people suffering from insomnia and reduce pain-catastrophizing in those with knee osteoarthritis.
When should you see a doctor for knee pain at night?
The most common cause of night-time pain in a knee is osteoarthritis but other conditions like nerve irritation, joint infection or carcinoma, can present in a similar fashion. If you are experiencing any of the following you should arrange to see your doctor:
- Your pain gets worse despite taking pain killers and trying self-help strategies
- Your sleep gets disturbed most nights of the week
- You notice swelling in or around the knee
- You develop a temperature along with your knee pain
- You are simply concerned
Disclaimer
This article is for information and educational purposes. Please note the date it was last reviewed or updated. Any content on this site, no matter when it was written, should never be used as a substitute to direct medical advice from your physician or other qualified health care provider.